Heal Your Heel
By Lynda Linforth
There are few things more frustrating than being mentally and physically committed to a new exercise program, only to be thwarted by injury. As Summer approaches and fitness enthusiasm turns more towards outside activities, I am prepared for the exuberant number of minor but hobbling injuries which clients will bring me by the beginning of the school holidays. The main injuries our clients come to work through are plantar fasciitis, Achilles tendonitis, knee, shoulder and lower back pain. This article will address plantar fasciitis and Achilles tendonitis.
A little pain in the ankle, Achilles tendon or foot can quickly escalate to huge problems if ignored. I had a client in my Bridal Boot Camp, desperate to lose weight for her wedding but both of her Achilles tendons started to give her pain. Assuming it was tendonitis, I restricted her impact workouts with bike riding only, upper body strength training and I changed her diet. Unbeknownst to me, she continued her nightly runs outside. The pain increased but her weight continued to drop. Her wedding was a fabulous event and she danced the night away in high heels. The next morning, when they were getting ready to leave on their honeymoon, she fell to the ground unable to walk. Her husband took her to the ER where an MRI showed both Achilles tendons had ruptured, needing immediate surgery. Instead of leaving for Italy that day, she spent the first 8 weeks of their marriage in a wheelchair recovering from surgery.
Plantar fasciitis is the painful inflammation of the fascia (fibrous connective tissue) around the plantar (sole of the foot but in this case, the heel). Many cases of heel pain are caused by inflammation which has been aggravated by a change in gait caused by the pain, inappropriate shoes, weight gain or increased impact activity. Most common symptoms are the intense pain felt when first stepping out of bed, heel tenderness when walking or exercising and knots or cramps in the arch of the foot.
I spoke with Craig Sapenoff, D.P.M. at Sapenoff & Harris Podiatry on Okeechobee Boulevard, West Palm Beach. Dr. Sapenoff treated me for a severe ankle sprain two years ago and I wanted to get his thoughts about heel pain in general. “While PF is the most common problem for heel pain symptoms, it’s not the only possibility. These symptoms are also seen with tarsal tunnel syndrome fracture, nerve entrapment and more.” Dr. Sapenoff said. Plantar fasciitis should be diagnosed by a medical professional before attempting treatment as similar symptoms occur for heel spurs and other pedalian complaints.
The most common causes of heel pain stem from steady weight gain followed by periods of inactivity followed by increased activity. This causes an unnatural load on the most sensitive part of the foot. However, athletes are not exempt. There are a high percentage of active people who suffer from repetitive injuries (tendonitis, bruising and plantar fasciitis) and especially those who partake in high impact activities such as running, and playing sports.
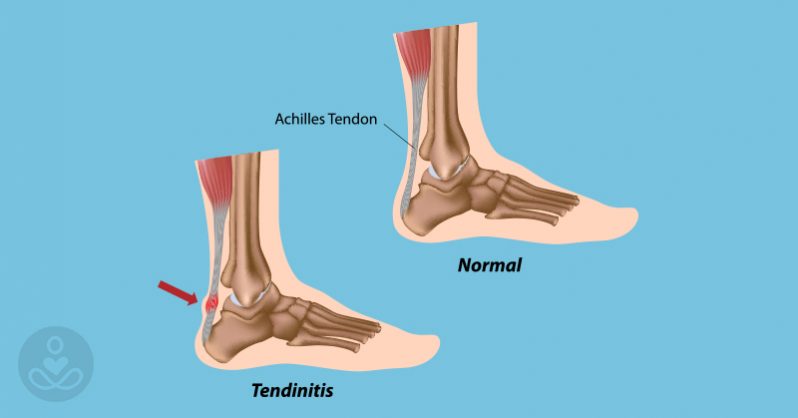
Achilles tendonitis can occur with or without plantar fasciitis but as they are in the same proximity (the Achilles tendon inserts in the calcaneus or heel bone) they are often present simultaneously.
Management: In regards to plantar fasciitis, ask your doctor about wearing a splint or boot-type support at night. This keeps your foot at a 90 degree angle during sleep to avoid that excruciating first step out of bed. Before leaving bed, try stretching out the hamstring (back of thigh) and the feet (by pulling your toes backwards). Step out of bed carefully, and gently lower your heel to the floor.
Shoe inserts such as orthotics or heel cups for everyday use can offer relief. Do not wear completely flat shoes as this will only aggravate the condition. Wear comfortable, slightly elevated shoes or tennis shoes. Absolutely NO flip-flops or any type of shoe that needs to be gripped by toes such as slides or mules. Do not partake in any impact activity and stretch calves and hamstrings daily or whenever they feel tight. Ice regularly as reducing the inflammation is critical to recovery. For Achilles pain, massage the calf muscles and minimize all activity which aggravates it (switching from running to cycling, for example). Ice regularly and rest as much as possible.